Certified Professional Coder (CPC) Exam Questions and Answers
A patient who is 37 weeks' gestation is admitted to labor and delivery for a cesarean delivery. An external cephalic version was performed successfully several days ago and she now presents in labor, fully dilated, and the fetus has returned to a footling presentation.
What anesthesia code is reported?
(A patient presents for surgery due to recurrent lumbar radiculopathy at a previously operated spinal level. The surgeon performs arepeat exploration laminotomywithbilateral foraminotomyto decompress nerve roots at theL1–L2 interspace. No additional spinal levels are treated. What CPT® coding is reported?)
A pediatrician is requested to attend a high-risk delivery and performs initial stabilization of the newborn after cesarean delivery.
What E/M service is reported?
In rhinoplasty:
According to the Application of Cast and Strapping CPT® guidelines, what is reported when an orthopedic provider performs initial fracture care treatment for a closed scaphoid fracture of the wrist, applies a short arm cast, and the patient will be returning for subsequent fracture care?
A patient undergoes a laparoscopic appendectomy for chronic appendicitis.
What CPT® and diagnosis codes are reported?
A physician conducts a 15-minute phone call discussing medication management.
How is this reported?
Provider performs staged procedures for gender reassignment surgery converting female anatomy to male anatomy.
What CPT® code is reported?
(A patient has nausea with several episodes of emesis and severe stomach pain due to dehydration. Normal saline is infused in the same bag with2 mg ondansetron. Then15 mg ketorolac tromethamineis given for stomach pain. What J codes are reported for these services?)
(Which CPT® code can append modifier50?)
A patient presents to the surgical suite for a planned sterilization procedure via a bilateral excisional vasectomy.
What is the correct CPT® code and diagnosis code for the service?
(When a provider’s documentation refers touse, abuse, and dependenceof the same substance (e.g., alcohol), which statement is correct?)
A provider orders liquid chromatography mass spectrometry (LC-MS) definitive drug test for a patient suspected of acetaminophen (analgesic) overdose. What CPT® code is reported for the test?
Which punctuation is used in the ICD-10-CM Alphabetic Index to identify manifestation codes?
(A patient suffering fromlateral epicondylitisin the left elbow is sent to the operating room tomanipulate the elbow. The patient is placed undergeneral anesthesiaby the anesthesiologist. The physician manipulates the elbow through stretching and rotation to restore motion. What CPT® coding is reported for the physician?)
A woman with vulvar intraepithelial neoplasia (VIN II) undergoes a partial vulvectomy (<80%) with removal of skin and deep subcutaneous tissue.
What CPT® and ICD-10-CM codes are reported?
(What CPT® coding is reported for the insertion ofHeyman capsulesfor clinical brachytherapy?)
The CPT® code book provides full descriptions of medical procedures, with some descriptions requiring the use of a semicolon (;) to distinguish among closely related procedures.
What is the full description of CPT® code 35860?
A planned partial meniscectomy of the temporomandibular joint is cancelled after anesthesia and incision due to respiratory distress.
What CPT® coding is reported for the oral surgeon?
A 50-year-old patient presented with a persistent cough has not responded to standard treatments. The patient's physician decides to perform a flexible bronchoscopy with bronchial biopsies to further investigate the cause. A flexible bronchoscope is inserted through the patient's mouth and into the bronchial tubes. Five biopsies are taken for further testing. The biopsies were sent to the lab for analysis to determine the next steps in the patient's treatment plan.
What CPT® coding is reported?
Which entity offers compliance program guidance to form the basis of a voluntary compliance program for a provider practice?
Ms. C is diagnosed with a supratentorial intracerebral hematoma, and the neurologist performs a craniectomy to access the hematoma. The hematoma is accessed, and a suction device is
used to remove it.
What CPT@ code is reported?
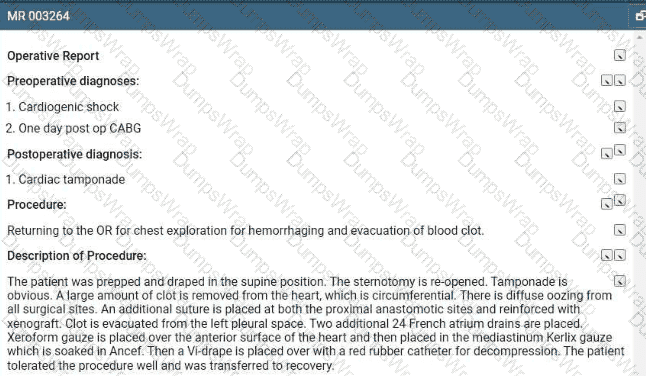
Refer to the supplemental information when answering this question:
View MR 003264
What is the procedural coding?
A male patient passes out while jogging in the park. Upon examination at the hospital, he is found to have a wide complex tachycardia and undergoes an electrophysiologic study and radiofrequency ablation. For this procedure he is placed under general anesthesia.
What is the anesthesia coding for this otherwise healthy 35-year-old?
Repeat three-view imaging of both hips and pelvis is performed on the same day due to a new fall, interpreted by the same radiologist.
What CPT® coding is reported?
A 53-year-old male arrived at the ER due to severe ocular trauma to the right eye. He was at work on a metal drilling machine and a metallic item penetrates his right eyeball. A foreign body is in
the posterior segment of the eye and corneal laceration with multiple posterior perforated sites were noted. He is brought back to the surgical suite. The surgeon removes the metallic foreign
body using large retinal forceps. The laceration of the cornea is sutured and the provider also performs a pars plana lensectomy.
What is the CPT® and ICD-10-CM codes are reported?
An abdominal X-ray includes decubitus, supine, and erect views.
What CPT® code is reported?
A patient underwent a colonoscopy, where the gastroenterologist biopsied two polyps from the colon. Each polyp was sent to pathology as separately identified specimens. The gastroenterologist was requesting a pathology consult while the patient was still on the table. Tissue blocks and frozen sections were then prepared and examined as follows:
Specimen 1: First Tissue Block—Three Frozen Sections Second Tissue Block—One Frozen Section Specimen 2: First Tissue Block—Two Frozen Sections Second Tissue Block—One Frozen Section
What CPT® coding is reported?
A patient in a radiology facility has an X-ray examination of her thoracolumbar junction due to pain while playing golf. The patient also has limited mobility in the hip. A radiologist takes a two view of the thoracolumbar junction.
What CPT® code is reported'
(A driver crashes into a guardrail and sustains a fracture of the anterior fossa cranial base with involvement of thesphenoid sinus, withno CSF leak. The patient undergoessurgical nasal sinus endoscopy with sphenoidotomyto evaluate and treat the sinus injury. No CSF leak repair is performed. What is the correct procedure and diagnosis coding combination to report this service?)
An established patient presents with fever and sore throat. Rapid strep test is positive.
What CPT® and ICD-10-CM codes are reported?
(A 6-month-old child was brought to the hospital with severe breathing difficulties. After testing, the child was diagnosed withtracheal stenosis present from birth. The pediatric surgeon performed atracheoplasty(surgical widening of the trachea). What CPT® and ICD-10-CM codes are reported?)
A child returns for stage 2 surgical repair of double outlet right ventricle, including removal of pulmonary artery band, arterial switch repair, and ECMO cannulation.
What CPT® codes are reported?
Which place of service code is submitted on the claim for a service that is performed in a skilled nursing facility?
A patient returns for embryo transfer. The lab thaws cryopreserved embryos and cultures them for two additional days.
What CPT® coding is reported?
A couple presents to the freestanding fertility clinic to start in vitro fertilization. Under radiologic guidance, an aspiration needle is inserted (by aid of a superimposed guiding-line) puncturing the ovary and preovulatory follicle and withdrawing fluid from the follicle containing the egg.
What is the correct CPT® code for this procedure?
(ESTABLISHED PATIENT VISIT: A 37-year-old woman presents with coughing, congestion, upper respiratory symptoms, and headache for two days. Complete ROS negative except as noted. No significant past/family history. Exam: stable vitals, nasal congestion, normal TMs, occasional rhonchi, no wheezing, normal heart, soft abdomen. Assessment/Plan:Acute upper respiratory infection, fluids,amoxicillinfor 5–7 days, return precautions. What CPT® code is reported?)
Refer to the supplemental information when answering this question:
View MR 065174
What E/M code is reported for this encounter?
(A 52-year-old woman has vulvar intraepithelial neoplasia (VIN II). The surgeon performs avulvectomyremovingless than 80%of the vulva, including affected skin and deep subcutaneous tissue. What CPT® and ICD-10-CM codes are reported?)
A patient with malignant lymphoma is administered the antineoplastic drug Rituximab 800 mg and then 100 mg of Benadryl.
Which HCPCS Level II codes are reported for both drugs administered intravenously?
An interventional radiologist performs an abdominal paracentesis using fluoroscopic guidance to remove excess fluid. The procedure is performed in the hospital. What CPT® coding is reported?
Miranda is in her provider's office for follow up of her diabetes. Her blood sugars remain at goal with continuing her prescribed medications.
When referring to the MDM Table in the CPT® code book for number and complexity of problems addressed at the encounter, what type of problem is this considered?
(An orthopedic surgeon evaluated a patient in the emergency room two months after a surgical repair of a right radius and ulnar shaft fracture. After reinjury, imaging shows a displaced proximal fixation screw andmalunion of only the radial shaft. The same surgeon performs surgery to repair the malunion using a graft from the hip. What CPT® and diagnosis codes are reported?)
Patient with erectile dysfunction is presenting for same day surgery in removal and replacement of an inflatable penile prosthesis.
What CPT® code is reported for this service?
A patient was in a car accident as the driver and suffered a concussion with brief loss of consciousness (15 minutes). What ICD-10-CM codes are reported?
A 65-year-old man had a right axillary block by the anesthesiologist. When the arm was totally numb, the arm was prepped and draped, and the surgeon performed tendon repairs of the right first, second, and third fingers. The anesthesiologist monitored the patient throughout the case.
What anesthesia code is reported?
Which one of the following activities, when performed, is NOT considered when selecting an E/M service level based on time?
A patient presents with fever, cough, SOB, and a recent history of COVID-19. A PCR test was positive for COVID-19. The provider documents a final diagnosis of “pneumonia with history of COVID-19.”
What ICD-10-CM coding is reported?
(A wheelchair-bound resident of a skilled nursing facility is seen in the physician’s office. The physician’s office makes arrangements with a social worker to take the patient back to the skilled nursing facility. What is the HCPCS Level II transportation service code?)
View MR 099401
MR 099401
Established Patient Office Visit
Chief Complaint: Patient presents with bilateral thyroid nodules.
History of present illness: A 54-year-old patient is here for evaluation of bilateral thyroid nodules. Thyroid ultrasound was done last week which showed multiple thyroid masses likely due to multinodular goiter. Patient stated that she can “feel" the nodules on the left side of her thyroid. Patient denies difficulty swallowing and she denies unexplained weight loss or gain. Patient does have a family history of thyroid cancer in her maternal grandmother. She gives no other problems at this time other than a palpable right-sided thyroid mass.
Review of Systems:
Constitutional: Negative for chills, fever, and unexpected weight change.
HENT: Negative for hearing loss, trouble swallowing and voice change.
Gastrointestinal: Negative for abdominal distention, abdominal pain, anal bleeding, blood in stool, constipation, diarrhea, nausea, rectal pain, and vomiting
Endocrine: Negative for cold Intolerance and heat intolerance.
Physical Exam:
Vitals: BP: 140/72, Pulse: 96, Resp: 16, Temp: 97.6 °F (36.4 °C), Temporal SpO2: 97%
Weight: 89.8 kg (198 lbs ), Height: 165.1 cm (65”)
General Appearance: Alert, cooperative, in no acute distress
Head: Normocephalic, without obvious abnormality, atraumatic
Throat: No oral lesions, no thrush, oral mucosa moist
Neck: No adenopathy, supple, trachea midline, thyromegaly is present, no carotid bruit, no JVD
Lungs: Clear to auscultation, respirations regular, even, and unlabored
Heart: Regular rhythm and normal rate, normal S1 and S2, no murmur, no gallop, no rub, no click
Lymph nodes: No palpable adenopathy
ASSESSMENT/PLAN:
1) Multinodular goiter - the patient will have a percutaneous biopsy performed (minor procedure).
What E/M code is reported for this encounter?
A patient has swelling in both arms and lymphangitis is suspected. She is in the outpatient radiology department for a lymphangiography of both arms.
What CPT® coding is correct?
A patient has suspicious lesions on his feet. Biopsies confirm squamous cell carcinoma. The patient elects to destroy a 0.6 cm lesion on the right dorsal foot and a 2.0 cm lesion on the left dorsal foot using cryosurgery.
What CPT® coding is reported?
A patient had surgery a year ago to repair two extensor tendons in his wrist. He is in surgery for a secondary repair for the same two tendons with free graft. What CPT® coding is reported?
A witness of a traffic accident called 911. An ambulance with emergency basic life support arrived at the scene of the accident. The injured party was stabilized and taken to the hospital. What HCPCS Level II coding is reported for the ambulance's service?
(Miranda is in her provider’s office for follow up of her diabetes. Her blood sugars remain at goal with continuing her prescribed medications. When referring to the MDM Table for number and complexity of problems addressed, what type of problem is this considered?)
(Which punctuation is used in the ICD-10-CM Tabular List to denotesynonyms, alternative wording, or explanatory phrases?)
(A three-year-old patient returns forstage 2treatment for double right outlet syndrome. The surgeon removes apulmonary artery bandand performstransposition repair of the great vesselsvia aortic pulmonary reconstruction. Central cannulae are inserted forECMO bypass, chemical cardioplegia is initiated, and a physician assistant monitors vitals and oxygenation until heart function resumes. What CPT® codes are reported for the surgery today?)
Which is a TRUE statement for Place of Service (POS) codes for professional claims?
A patient presents to the office with dysuria and lower abdominal pain. The physician suspects she has a UTI. A non-automated urinalysis is done in the office and is negative. UTI is ruled out
for the final diagnosis.
What CPT and ICD-10-CM codes are reported?
A 55-year-old patient was recently diagnosed with an enlarged goiter. It has been two years since her last visit to the endocrinologist. A new doctor in the exact same specialty group will be examining her. The physician performs a medically appropriate history and exam. The provider reviewed the TSH results and ultrasound. The provider orders a fine needle aspiration biopsy which is a minor procedure.
What E/M code is reported?
Which one of the following is correct to report an intermediate repair code (12031–12037)?
Which one of the following terms refers to inflammation of the liver?
From a left femoral access, the catheter is placed within the proper hepatic artery, dye is injected, and imaging is obtained. A stenosis within this artery is identified. A percutaneous
transluminal angioplasty is performed on the proper hepatic (visceral) artery in the outpatient radiology department.
What CPT® coding is reported?
A patient with a history of chronic venous embolism in the inferior vena cava has a radiographic study to visualize any abnormalities. In outpatient surgery the physician accesses the subclavian vein and the catheter is advanced to the inferior vena cava for injection and imaging. The supervision and interpretation of the images is performed by the physician.
What codes are reported for this procedure?
(A patient with abnormal growth had asuppression studythat includedfive glucose testsandfive human growth hormone tests. What CPT® coding is reported?)
A 5-year-old patient has a fractured radius. The orthopedist provides moderate sedation and the reduction. The time is documented as 21 minutes.
What CPT® code is reported for the moderate sedation?
A patient's left eye is damaged beyond repair due to a work injury. The provider fabricates a prosthesis from silicon materials and makes modifications to restore the patient's cosmetic appearance.
What CPT® code is reported?
Which statement is FALSE in reporting a personal history ICD-10-CM code?
A physician sees a patient for the first observation visit, spends 85 minutes, with moderate MDM.
What CPT® code is reported?
A patient arrives with stridor and in respiratory distress. The provider performs a micro laryngoscopy using a Parson's laryngoscope and magnifying telescope. A bronchoscopy was also
performed using a 2.5 Stortz bronchoscope. The findings include subglottic web and stenosis with laryngeal edema suggestive of reflux. There was also significant collapse of the trachea at
the carina and into the main bronchi bilaterally.
What CPT® coding is reported?
A catheter was placed into the abdominal aorta via the right common femoral artery access. An abdominal aortography was performed. The right and left renal artery were adequately visualized. The catheter was used to selectively catheterize the right and left renal artery. Selective right and left renal angiography were then performed, demonstrating a widely patent right and left renal artery.
What CPT® coding is reported?
A 42-year-old male is diagnosed with a left renal mass. Patient is placed under general anesthesia and in prone position. A periumbilical incision is made and a trocar inserted. A laparoscope is inserted and advanced to the operative site. The left kidney is removed, along with part of the left ureter. What CPT® code is reported for this procedure?
Eric is buying his first life insurance policy from XYZ Life Insurance Company. The company requires Eric have a physical exam prior to issuance of the policy. Eric sees his primary care provider who completes the required documentation and forms provided by the insurance company.
How does the primary care provider report his services?
A patient with end-stage renal disease (ESRD) receives hemodialysis 3x weekly in the office for one month. The nephrologist performs a comprehensive exam and supervises dialysis.
What CPT® and ICD-10-CM codes are reported?
A physician orders an obstetric panel that includes syphilis screening using the non-treponemal antibody approach, an automated CBC with manual differential WBC count, HBsAg, rubella antibody, a serum antibody screen, and ABO and Rh blood typing.
What CPT® coding is reported?
What is the medical term for a procedure that creates an opening between the bladder and the rectum?
(The patient presents to the emergency department with chest pain. EKG showsNSTEMIand troponin is abnormal. The ED provider discusses the case with a cardiologist and the patient is admitted for heart catheterization/PCI. What is the E/M service and ICD-10-CM coding reported for the ED provider?)
A 64-year-old with congestive heart failure (CHF) has pericardial effusion. The provider inserts a needle under ultrasound guidance, aspirating the fluid from the pericardial sac.
What CPT® coding is reported?
A patient presents to the pulmonologist's office for the first time with coughing and shortness of breath. The patient has a history of asthma. The physician performs a medically appropriate
history and exam. The following labs are ordered: CBC, arterial blood gas, and sputum culture. The pulmonologist assesses the patient with a new diagnosis of COPD. The patient is given a
prescription for the inhaler Breo Ellipta.
What E/M code is reported?
A 67-year-old male presents with DJD and spondylolisthesis at L4-L5 The patient is placed prone on the operating table and, after induction of general anesthesia, the lower back is sterilely prepped and draped. One incision was made over L1-L5. This was confirmed with a probe under fluoroscopy. Laminectomies are done at vertebral segments L4 and L5 with facetectomies to relieve pressure to the nerve roots. Allograft was packed in the gutters from L1-L5 for a posterior arthrodesis. Pedicle screws were placed at L2, L3, and L4. The construct was copiously irrigated and muscle; fascia and skin were closed in layers.
Select the procedure codes for this scenario.
A patient is seen at the doctor's office for nausea, vomiting, and sharp right lower abdominal pain. CT scan of the abdomen is ordered. Labs come back indicating an increased WBC count with
review of the abdominal CT scan. The physician determines the patient has chronic appendicitis. The physician schedules an appendectomy and takes the patient to the operating room. The
appendix is severed from the intestines and removed via scope inserted through an umbilical incision. What CPT® and diagnosis codes are reported?
A surgeon performs a complete bilateral mastectomy with insertion of breast prosthesis at the same surgical session.
What CPT@ coding is reported?
An incision is made in the scalp, a craniectomy is performed to access the area where electrodes are present. The electrodes are removed. The surgical wound is closed.
What procedure code is reported?
What does the suffix -graph mean?
An otolaryngologist performs a tympanoplasty with mastoidectomy, reconstruction of the posterior ear canal wall, and ossicular chain reconstruction.
What CPT® code is reported?
A patient with suspected gynecologic malignancy undergoes laparoscopic staging including bilateral pelvic lymphadenectomy, periaortic lymph node sampling, peritoneal washings, peritoneal and diaphragmatic biopsies, and omentectomy.
What CPT® coding is reported?
(Preoperative diagnoses:Bradycardia.
Postoperative diagnosis:Bradycardia.
Procedure performed:Dual-chamber pacemaker implantation.
Brief history:77-year-old female with recurrent syncope; evaluation revealed first-degree AV block, sinus bradycardia, bundle-branch block; bradyarrhythmia suspected; after discussion with her sister, dual-chamber pacemaker recommended; risks explained; consent obtained.
Procedure details:Taken to cardiac catheterization lab; positioned on cath table; prepped/draped standard; procedure challenging due to agitation despite adequate sedation; left infraclavicular area anesthetized with 0.5 cc Xylocaine; pacemaker pocket created; hemostasis with cautery; 9-French peel-away sheath used to introduce an atrial and a ventricular lead; leads positioned with excellent thresholds; secured with O-silk sutures over sleeves; pulse generator connected; pocket flushed with antibiotic solution; pacemaker/leads placed in pocket; incision closed in two layers; performed under fluoroscopic guidance.
Complication:None.
Plan:Return to recovery; discharge later this evening to nursing home with routine post-pacemaker care.
Question:What CPT® coding is reported for this procedure?)
Day 1 - A provider admits the patient to observation care for type 2 diabetes mellitus with hyperglycemia. The provider orders a HbA1c, a urine (microalbumin), and kidney function lab tests.
Blood sugar is high and poorly controlled. The provider discusses the case with the patient's endocrinologist. The provider prescribes an IV insulin drip, along with SQ insulin and keeps the
patient in observation overnight.
Day 2 - Patient is in observation care and the provider orders a blood glucose test. The patient's glucose levels have improved. The provider places an order for the dietitian to see the patient.
Provider
documents spending a total time of 25 minutes with the patient.
Day 3 - Patient has a blood glucose test. The patient's glucose level is back to normal. The provider documents spending 15 minutes with the patient. The provider discharges the patient.
What E/M coding is reported by the physician for the patient in observation care?
A CRNA independently administers MAC anesthesia for ICD replacement.
What CPT® and ICD-10-CM codes are reported?
A patient arrives at the clinic experiencing pain due to a chest injury caused by blunt force. The provider takes X-ray imaging with 6 views of the chest.
What CPT® coding is reported?
(A 62-year-old with insulin-dependent diabetes mellitus has sudden hearing loss. The otolaryngologist administered atranstympanic injection of a steroidfor the sudden hearing loss ineach ear. How is this reported?)
What does the term “manipulation” refer to in the context of fracture or dislocation treatment?
A patient is going to have placement of a myringotomy tube. This tube is placed in the ______ to drain excess fluid.
A healthy 35-year-old undergoes EP study and ablation under general anesthesia.
What anesthesia coding is correct?
(Which one of the following is an anesthesiaphysical status modifier?)
Which statement is NOT true regarding the ICD-10-CM coding guidelines for burns?
A 58-year-old with type 1 diabetes mellitus comes in for comprehensive eye examination. She is diagnosed with diabetic retinopathy with macular edema in the right eye. What ICD-10-CM coding is reported?
A patient with compression fractures of L5 and the sacrum undergoes vertebroplasty, with cement injected into two vertebral bodies, performed bilaterally.
What CPT® coding is reported?
(A patient is seen for nausea, vomiting, and sharp right lower abdominal pain. CT and labs support a diagnosis ofchronic appendicitis. The physician schedules anopen appendectomyand removes the appendix. What CPT® and diagnosis codes are reported?)
The Medicare program has multiple parts covering different services. Which part provides coverage for outpatient physician charges?
Ten-year-old boy has a painful felon abscess of the deep tissues of the palmar surface of his right thumb. The provider makes an incision on one side of the nail and then across the fingertip parallel to the end of the nail. He identifies the area of abscess and drains it. A drainage tube is inserted.
What CPT® and ICD-10-CM is reported?
A 44-year-old female patient came in for a planned laparoscopic total abdominal hysterectomy for endometriosis of the uterus. The surgeon attached the trocars, a scope is inserted examining
the uterus, abdominal wall, bilateral ovaries, and fallopian tubes. The surgeon decided to convert the laparoscopic procedure to an open total hysterectomy because of the extensive amount of
adhesions that need to be removed. A total hysterectomy was performed and due to removal of the extensive adhesions the surgery took longer than normal of 2 hours.
What CPT® and diagnosis codes are reported?
Four malignant peritoneal tumors are excised, the largest measuring 15 cm.
What CPT® and ICD-10-CM coding is reported?
A patient is diagnosed with a healing pressure ulcer on her left heel that is currently being treated.
What ICD-10-CM coding is reported?
(Full Case:Preoperative diagnosis:Low back pain; possible spinal stenosis L3–4.Postoperative diagnosis:No evidence of discogenic pathology or spinal stenosis at L3–4; normal discography L3–4.Procedure:Awake discography and injection, L3–4.Anesthesia:IV narcotic with reversal and local; propofol given transiently, then patient alert/responsive for pain response during injection.Technique:Patient to OR; right decubitus; sterile prep/drape; C-arm used to mark entry; local ethyl chloride + 1% Xylocaine; docking needle placed posterolateral at L3–4 under AP/lateral; inner needle advanced to disc nucleus center; contrast injected while monitoring patient response; normal bilocular pattern; 1.5 cc volume; no pain with pressurization.Documentation:No videotape; plain films available; post-discography CT planned/reviewed for other causes.Question:What CPT® and ICD-10-CM coding is reported?)
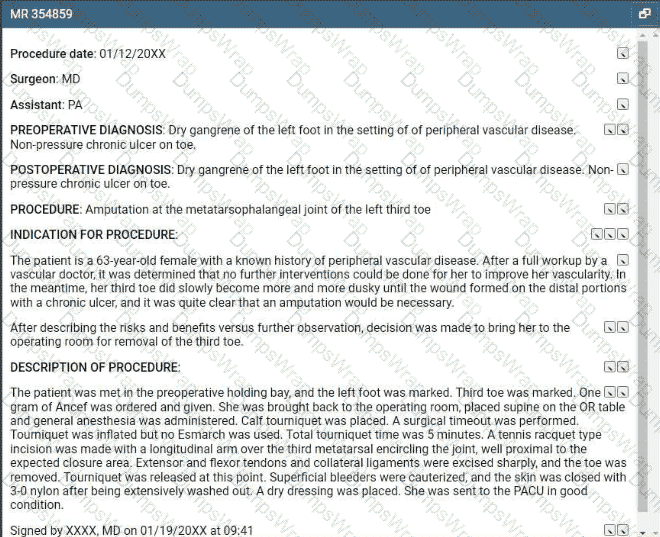
Refer to the supplemental information when answering this question:
View MR 354859
What CPT® and ICD-10-CM coding is reported?
A 47-year-old male recently injured as a passenger in a car accident sustained multiple fractures. The patient now has physical restraints due to pulling out foley catheter, IV catheters and
attempted to pull out NG tube. Emergency department physician is asked to come see patient and injects 0.5 lidocaine into lumbar region of the spine. An indwelling catheter is placed into the
lumbar region for continuous infusion with fluoroscopy for pain management.
What CPT® is reported for the Emergency department physician?
(A 3-year-old is seen by his primary care physician for anannual exam. His last exam with the primary care physician wastwo years ago. He has no complaints. What CPT® code is reported?)
(What is the ICD-10-CM code for amedial meniscus tearof theleft kneedue to arecent football injury?)
(Which of the following is classified ascoronary arteries?)
A patient arrives for a PEG placement. The patient requires tube feeds for nutrition but frequently pulls out the dobhoffs tube. An EGD was performed. Several attempts were made to place the
PEG tube without success so the procedure was aborted. During the withdraw of the scope, a small hiatal hernia was noted in the stomach. The scope was removed the the patient transferred
to recovery.
What CPT and ICD-10-CM coding is reported?
(A 58-year-old patient undergoes diagnostic facet joint injections. The physician performsbilateral paravertebral facet joint injectionsat theT2–T3, T3–T4, and T4–T5levels, usingfluoroscopic guidanceat each site. What CPT® coding is reported for this encounter?)
(A 32-year-old visited a provider due to ongoing irritation and watering in his left eye. Suspecting an allergy, the provider carried out a test, introducing an allergenic extract into the mucous membrane inner lining of the eye. The patient’s eye is monitored for signs of an allergic reaction, such as redness and itching. What CPT® code is reported?)
A 19-year-old is seen by his, primary care physician for an annual exam. His last exam with the primary care physician was four years ago. He has no complaints.
What CPT code is reported?
A 74-year-old arrived at the ED experiencing bright red rectal bleeding when using the toilet. She does not have any abdominal pain, no nausea or vomiting. She has been undergoing dialysis for
years due to end-stage renal failure and has a diagnosis of myelodysplastic syndrome with a platelet count of just 3,000. Her hemoglobin level, which was 10 at her dialysis session the
previous day, dropped to 7. Abdominal films are negative. An urgent esophagogastroduodenoscopy (EGD) was performed, and no active bleeding was found in the esophagus or the stomach.
However, the scope was passed into the upper duodenum which did reveal some oozing, and was controlled with cautery. Next, the patient was then positioned on her left side for a
colonoscopy that extended from the colon to the ileum and into the lower duodenum, but no definitive sources of bleeding were found. Again, no outright bleeding sources were identified. A
CRNA performed the anesthesia and documented PS III.
What CPT® codes are reported for the CRNA?
(A 40-year-old woman with progressive sensorineural hearing loss in the right ear has acochlear implantplaced for the right ear. Anesthesia is provided by aCRNAwithmedical directionby an anesthesiologist who is concurrently directing 5 CRNAs. Physical status is3. What anesthesia CPT® and ICD-10-CM codes are reported by theanesthesiologist?)
(A patient is in her otolaryngologist’s office to receive therapeutic treatment forasthmatic bronchitis with status asthmaticus. A subcutaneous injection ofomalizumab (150 mg)is given in her left upper arm. What is the CPT® and ICD-10-CM coding?)
A patient has a 5 cm tumor in the left lower quadrant abdominal wall, excised through dermis and subcutaneous tissue. Pathology is pending to rule out cancer.
What CPT® and ICD-10-CM codes are reported?
(A 65-year-old male patient passed away due to unknown causes. An autopsy was ordered by the attending physician to determine the cause of death. The pathologist performed agross and microscopic examination autopsy, that includes thebrain and spinal cord. What CPT® coding is reported?)
A suppression study includes five glucose tests and five growth hormone tests.
What CPT® coding is reported?
(Procedure date:01/12/20XX
Surgeon:MD |Assistant:PA
Preoperative diagnosis:Dry gangrene of the left foot in the setting of peripheral vascular disease. Non-pressure chronic ulcer on toe.
Postoperative diagnosis:Dry gangrene of the left foot in the setting of peripheral vascular disease. Non-pressure chronic ulcer on toe.
Procedure:Amputation at the metatarsophalangeal joint of the left third toe
Indication:63-year-old female with peripheral vascular disease; vascular workup determined no further interventions to improve vascularity; third toe became progressively dusky; wound formed distally with chronic ulcer; amputation necessary; risks/benefits discussed.
Description:Left foot and third toe marked; 1 g Ancef given; general anesthesia; supine; calf tourniquet; timeout; tourniquet inflated (no Esmarch); total tourniquet time 5 minutes; tennis racquet incision with longitudinal arm over third metatarsal encircling joint proximal to closure; extensor/flexor tendons and collateral ligaments excised sharply; toe removed; tourniquet released; superficial bleeders cauterized; washed out; skin closed with 3-0 nylon; dry dressing; to PACU in good condition; signed 01/19/20XX 09:41.
Question:What CPT® and ICD-10-CM coding is reported?)
A catheter is placed from the femoral artery into the right common carotid, with imaging of the ipsilateral extracranial carotid and bilateral external carotids.
Which CPT® codes are reported?
(In the ICD-10-CM code book, which instructional note given in the Tabular List indicates whentwo conditions cannot be reported together?)
A patient suffers a ruptured infrarenal abdominal aortic aneurysm requiring emergent endovascular repair. An aorto-aortic tube endograft is positioned in the aorta and a balloon dilation is performed at the proximal and distal seal zones of the endograft. The balloon angioplasty is performed for endoleak treatment.
What CPT® code does the vascular surgeon use to report the procedure?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® coding is reported?
A provider performs a mastoidectomy and complete labyrinthectomy for right-sided peripheral vertigo.
What CPT® and ICD-10-CM codes are reported?
When a provider's documentation refers to use, abuse, and dependence of the same substance (e.g. alcohol), which statement is correct?
Patient is diagnosed with dacryocystitis, which is the inflammation of?
A flexible sigmoidoscopy is performed with ablation of two sigmoid colon polyps.
What CPT® and ICD-10-CM codes are reported?
The human shoulder is made of which three bones?
The gastroenterologist performs a simple excision of three external hemorrhoids and one internal hemorrhoid, each lying along the left lateral column. The operative report indicates that the internal hemorrhoid is not prolapsed and is outside of the anal canal.
What CPT® and ICD-10CM codes are reported?
A patient undergoes a percutaneous liver biopsy with ultrasound guidance for primary biliary cirrhosis.
What CPT® and ICD-10-CM codes are reported?
(A patient is diagnosed with agangrenous ulceron theright thighwith thefat layer exposedand is currently being treated. What ICD-10-CM coding is reported?)
A 4-year-old, critically ill child is admitted to the PICU from the ED with respiratory failure due to an exacerbation of asthma not manageable in the ER. The PICU provider takes over the care of the patient and starts continuous bronchodilator therapy and pharmacologic support with cardiovascular monitoring and possible mechanical ventilation support.
What is the E/M code for this encounter?